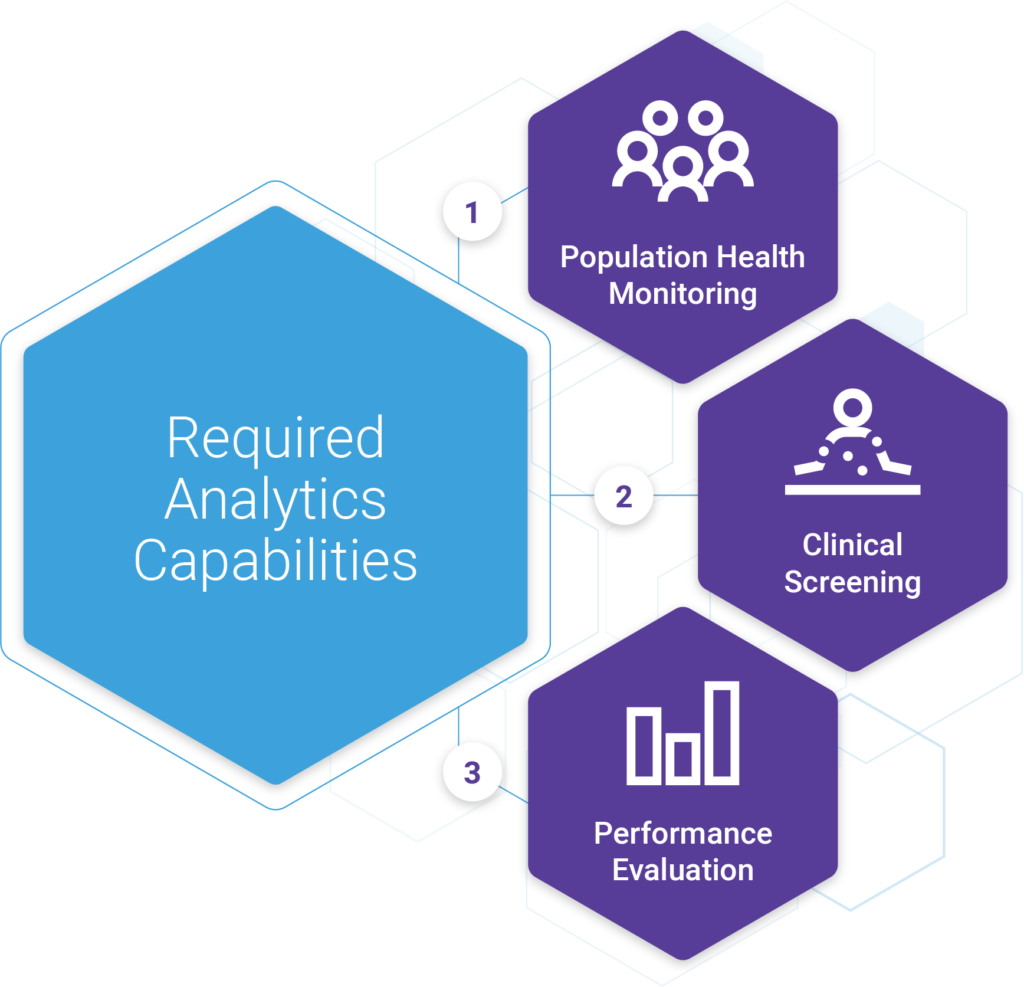
In part 3 of this blog series, we outlined three critical capabilities needed in any population-based care management analytics platform. They were,
- Population health monitoring
- Clinical screening
- Performance measurement
Over the next several blogs, we’ll break down each of these areas in more detail kicking things off with population health monitoring.
What is Population Health Monitoring?
Population health monitoring sometimes referred to as population health surveillance, is the ongoing systematic collection, analysis, interpretation, and dissemination of data to those responsible for preventing and controlling disease and injury.
The whole goal of population health monitoring is to ensure that organizations have the information and tools required to better understand the needs of their patients so that they can deliver the appropriate care and connect them with the necessary resources and services.
An important concept in population health monitoring is the idea that the level of resources necessary for delivering appropriate healthcare is correlated with the illness burden of that population. Therefore, it’s vital that clinicians better understand morbidity patterns and the burden of illness, so that they can design initiatives to best meet those needs of each targeted group of patients.
Effective population health monitoring is accomplished in four steps: Identifying patients, tracking their experience, assessing their risk, planning appropriate interventions.
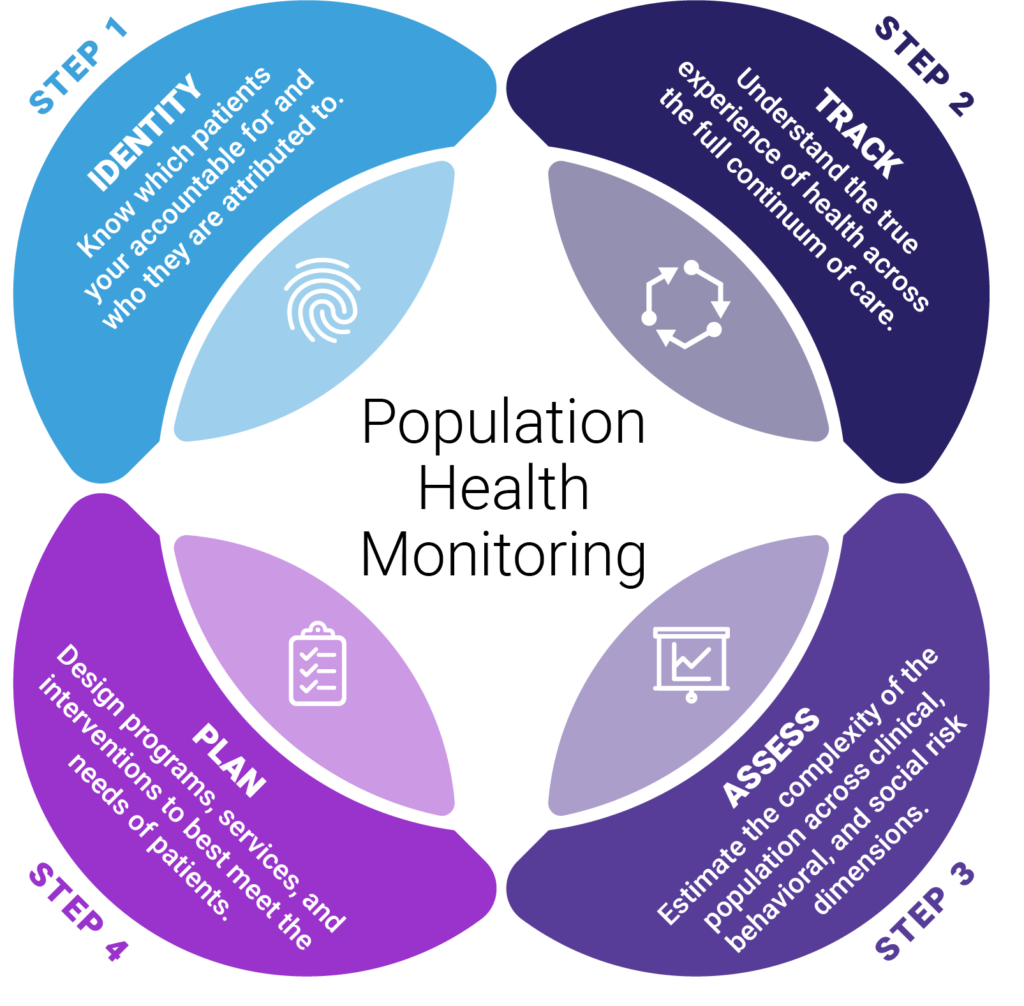
Population Health Monitoring, Step 1: Identification
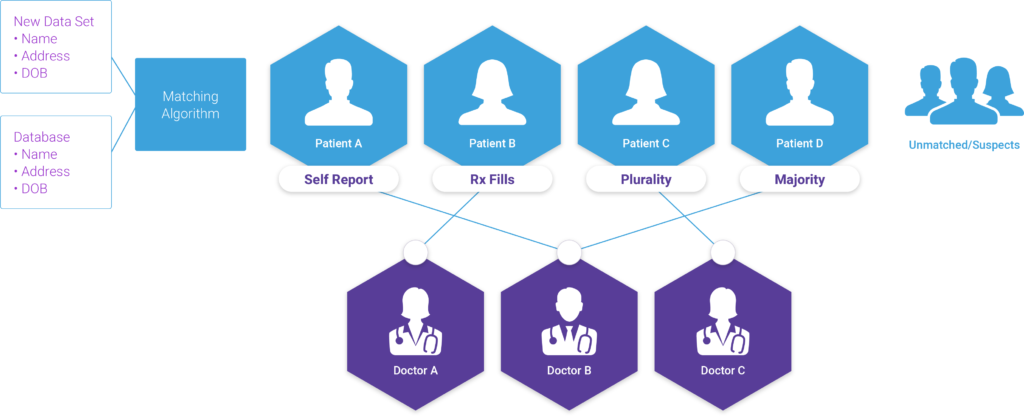
The first step in knowing your population is identifying which patients are yours. This involves two major activities: (1) identity management and (2) attribution. After conducting these steps, the population health team should aim to have three groups:
- Matched member/patient records that are accurately assigned to an active Primary Care Provider (PCP).
- Matched member/patient records that need to be assigned to an active PCP.
- Unmatched member/suspect records that require follow-up with the payer.
Identity Management
A typical scenario kicks off, with a member of the population health team collecting rosters from each payer’s portal (or some other mechanism for securely retrieving these lists); which is usually done on a monthly or quarterly basis. The population health team collects the rosters, most often via CSV, and then compares it to the export of patient records from the EHR. Vlookups are run to identify matches across the lists, with the goals of identifying members who (1) match up to existing patient records vs (2) those that require further research.
Members that can’t be matched are investigated one by one through the EHR. Members that fall into this bucket once, typically end up in this bucket every time. This requires the population health team to maintain a “Master list” that is used to track which members have been reconciled in previous months and which ones haven’t, in order to avoid unnecessary re-work. Reconciling flat files in this way is certainly doable, but with messy data, duplicate records, and missing patient information it can quickly become very resource-intensive, time-consuming, and prone to error.
Attribution
Even after all of that, there’s the added step of verifying that the patient is attributed appropriately. These activities include working through the list of “matched” records to confirm that they are accurately assigned to an active Primary Care Provider (PCP) within the group practice. This includes looking for deceased patients; patients assigned to PCPs that have left the group; patients attributed based on services received at an Urgent Care clinic; etc. Once these groups are reconciled, then the care team can turn their attention to more nuanced records e.g., multiple care providers treating the same patients, patients that are unresponsive to outreach or scheduling, etc.
Attribution methodology is at the core of constructing actuarially sound, provider-accepted and operational Alternative Payment Models (APMs), and attribution is the most critical component of valuebased contract design – Society of Actuaries (SOA)
5 Capabilities to Streamline Identification
Depending on the number of lives the organization is accountable for and how mature their capabilities are, reconciliation can take anywhere from 1 to 3 days for a single FTE. Selecting the right integrated data and analytics platform can significantly improve efficiency and reduce the time needed to reconcile these reports. We’ve compiled a list of the top five features. They are,

1 – Flexible Attribution Models
Each payer will have its own unique model for assigning patients to PCPs. These can range from basic to highly complex. Similarly, each provider group will have its own unique way of verifying the patient/provider relationship. Therefore, it’s critical to invest in technology that is flexible and can accommodate various models and formats to align with organizational processes.
2 – Patient Matching & Indexing
Understanding each patient’s healthcare journey requires data from many different sources. Integrating data in this way requires robust patient matching and indexing capabilities. A well-designed care management platform will include a master patient indexing system that assigns a unique identifier to each patient and then matches other sources (e.g., claims, membership, etc.) to that patient record.
3 – Manual Verification & Master List Management
Having to re-verify member/patient matches for the same individual each month is cost-prohibitive and unnecessary. A care management analytics platform that allows users to manually verify a match/non-match and retain that month over month until a patient’s details change is critical to streamlining the Identification workflow and avoiding the need to retain a “master list”.
4 – One-to-Many Relational Design
Taking a patient-centered approach to care delivery requires a patient-centered approach to analytics. It’s important that a care management platform track a patient’s journey over time, even when they change insurance carriers or products. this requires the ability to match many membership records to a single patient record without losing the historical context.
5 – Historical Record Keeping
It’s important to know which PCP is accountable both concurrently and retrospectively for many reasons. Taking a snapshot of attribution each month and tracking that quarter by quarter and year over year, can be incredibly powerful in assessing provider performance and identifying high-value care opportunities.
What’s Next?
Check out our upcoming blog as we continue to examine the steps of population health monitoring, where we’ll take a deep dive into building the 360-degree patient view and what that means for understanding a patient’s healthcare journey across the continuum of care. To learn more about Inflight Health Identity Management and Attribution solutions, contact a member of our Success team.