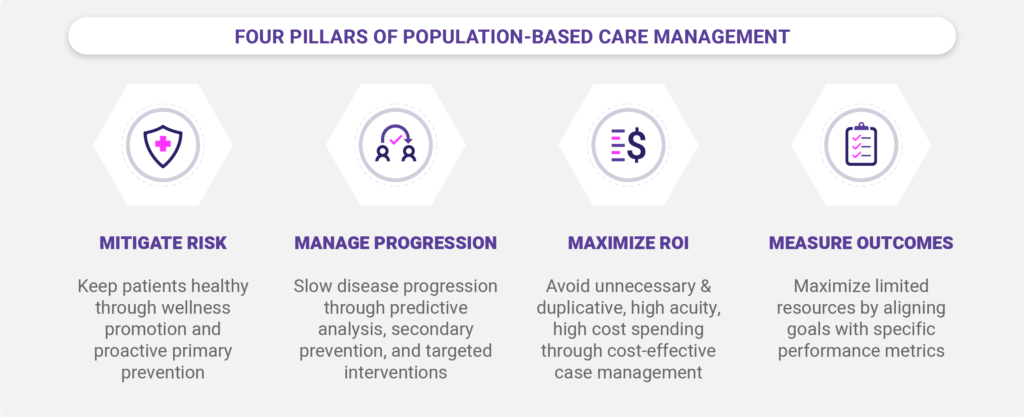
In blog 1 of this series, we discussed the importance of taking a population-based approach to care management, with the goal of keeping patients healthy and slowing the progression of disease.
Recall that a population-based care management approach applies care services across the full continuum of health, for ALL patients, with the aim of providing appropriate interventions based on the individual’s current health status and unique needs.
A Growing Strategic Focus on Integrated Systems
In the context of a population-based approach, care management is extremely broad and covers a wide range of activities. These activities include outreach, education, risk capture, gap closures, care/transitions/referral coordination, disease prevention & intervention, as well as acute case management for medically and behaviorally complex patients.
Achieving both clinical and financial success under this type of model requires a well-designed care management framework powered by integrated data, predictive analytics, insightful reports/visuals, in a secure and compliant platform.
With the right tools and information, clinicians can efficiently carry out the activities of population health management, including Identifying opportunities to better manage populations; understanding risk factors to deliver personalized medicine; predicting patients that are likely to experience adverse health outcomes and high costs of care; evaluating if variations are correlated to patient complexity or the way medicine is being practiced; supporting equitable rate setting in value-based payment structures.
Three Must-Have Capabilities in a Care Management Solution
A well-designed integrated data and analytics platform will support three functional capabilities of care delivery, which are described briefly below. We’ll explore these concepts in more detail in our upcoming blogs, as part of this series.
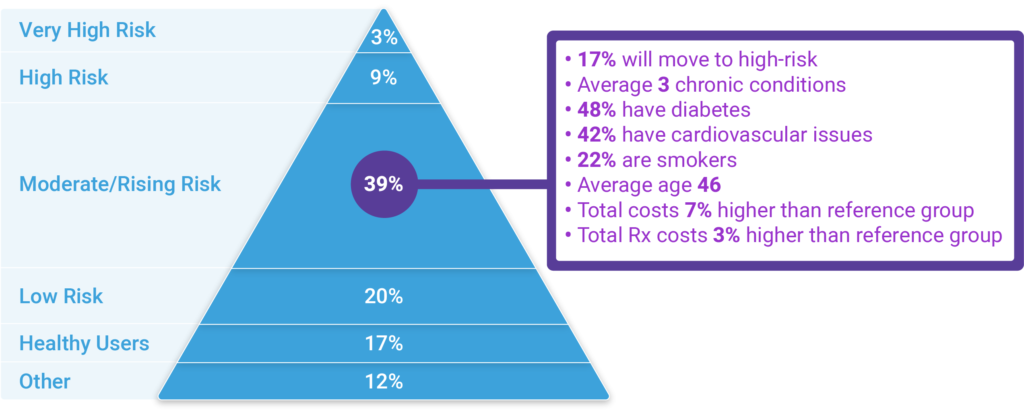
Population health monitoring
Knowing the population is the fundamental first step towards improving health and slowing the progression of the disease. With stratification and segmentation capabilities, clinicians can better understand the burden of illness, and more importantly, design initiatives to best meet those needs of each targeted group of patients while making the best use of limited resources.
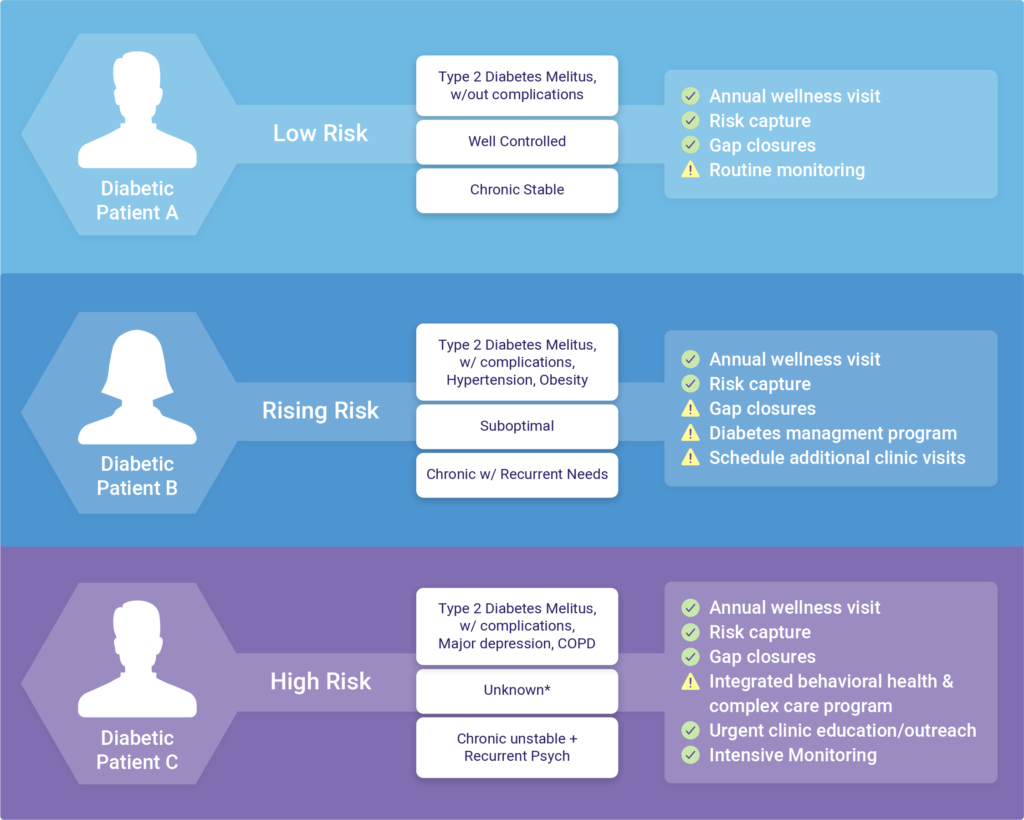
Clinical screening & prioritization
Once programs & interventions are prioritized, based on the needs of the population, the next step is to assign individual patients to intervention pathways. This assignment should be based on several dimensions of risk, including but not limited to: health status predicted costs/resource use, and other markers such as the probability of inpatient hospitalization, unique providers have seen, gaps in prescription refills, chronic condition count, functional status, etc.
Performance evaluation
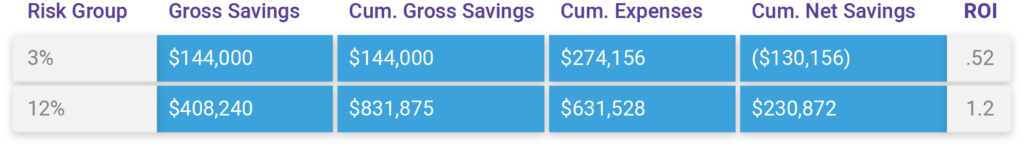
Once programs are implemented it is important to understand how successful it was and whether or not it should be altered or retired. It’s also important to understand the engagement and graduation rates for individuals to quantify improved outcomes and total per capita health care savings. This information is not only important for network and public reporting/transparency but also to identify characteristics associated with success to elevate future risk scoring capabilities.
Stay with us, as we explore these functional capabilities in more detail in our upcoming blogs. For immediate questions or inquiries about capabilities and solutions at Inflight Health, you can contact a member of our success team.