Health care delivery systems across the United States are focused on improving the health of populations through better care and smarter spending. Over this past decade, proactive care management has emerged as a leading strategy to achieve these goals.
What is Care Management?
Care management is a collaborative, team-based, patient-centered approach to care delivery that’s focused on helping patients achieve holistic health & wellness through improved care planning, coordination, and patient engagement based on the individual’s specific needs and health status.
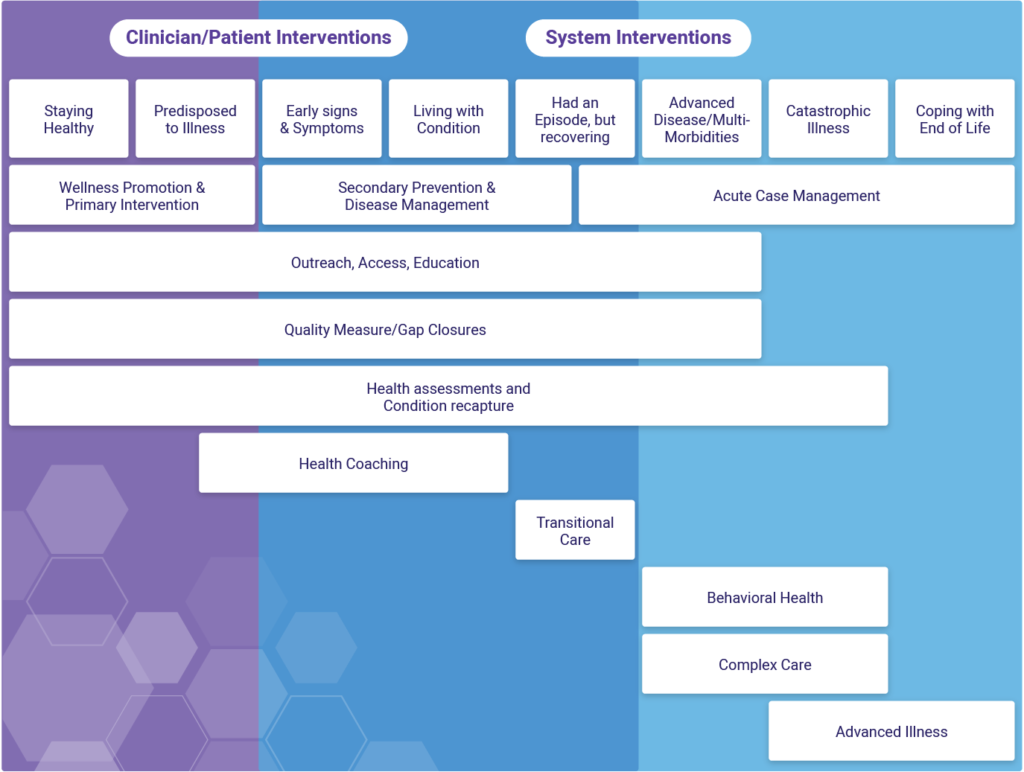
Care management programs manifest in many ways, (i.e., organizational goals, strategies, target populations, specific services provided or emphasized, administrative practices, and assessment capabilities) and encompass a wide range of activities performed at the clinician and system levels.
Challenges in Sustaining Care Management Systems
Despite care management’s growing popularity and widespread adoption, questions remain on how to best optimize and pay for the mix of staff, services, and infrastructure required for its delivery; especially during this very slow transition away from fee-for-service (FFS) payment structures towards value/risk-based contracts.
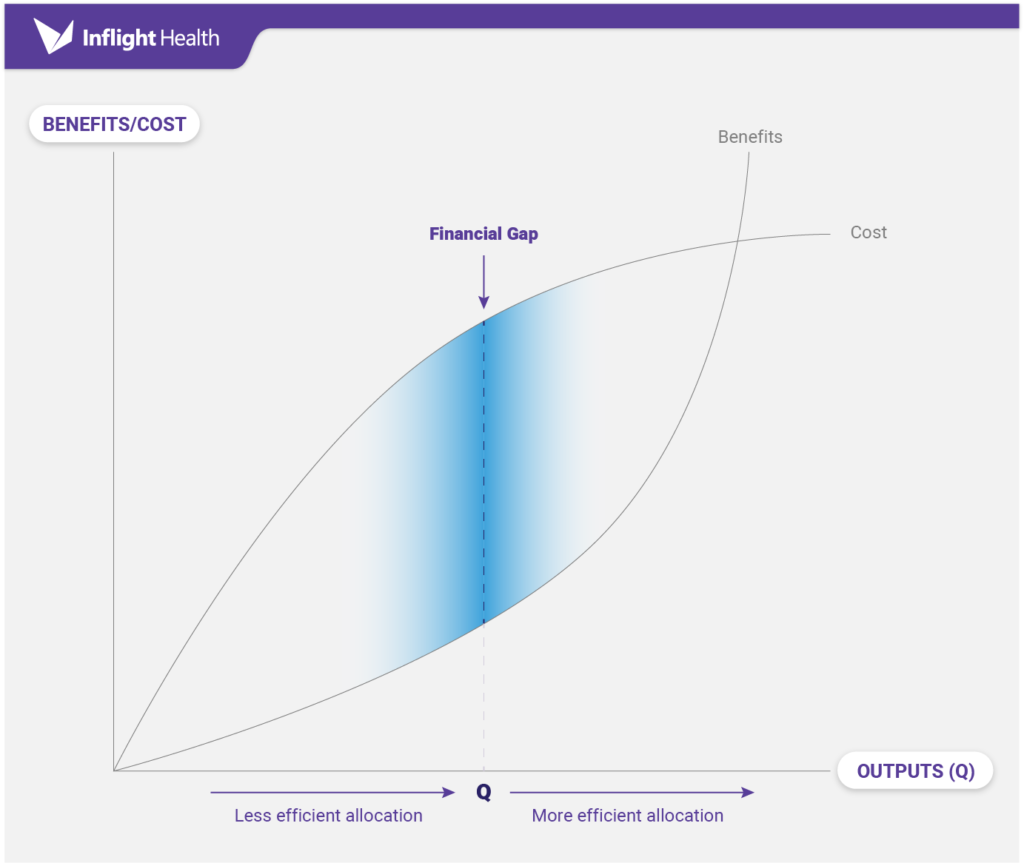
Because most traditional FFS models don’t reimburse practices for these activities, we’re seeing providers approach care management in a very limited capacity by focusing strictly on high-risk, high-cost value-based lives. While this might appear to be a fiscally responsible approach towards limiting the “Financial gap” associated with care management, experts would argue that these tactics actually hinder cultural and transformational progress towards value-based care, creating isolated efforts that don’t scale and lead to inefficient practices that prohibit future growth opportunities.
Keys to Overcoming These Challenges
Unfortunately, there is just no easy answer to these questions. The only thing that can help limit the growing pains associated with transformation is getting through it as fast as possible by acquiring as much risk as possible as quickly as possible. This no doubt will require a drastic cultural, financial, and clinical shift and executives will need to be prepared to lead their teams through this very difficult transition period.
Organizations that have managed to make this jump successfully tend to exhibit three common characteristics: (1) They take a very resource lean approach by repurposing existing resources, as opposed to investing in new ones; (2) They invest in integrated data and predictive analytics capabilities to truly understand their population’s needs and separate out the financials so they can see what’s going into and coming out of their contracts; (3) They take a population-based approach to care management which includes their full patient population, not just those high-risk, high-cost value-based lives.
Achieving Population Health by Maintaining a Long-term Focus
In a world where most people play the short game, playing the long game offers a huge advantage. While it might seem risky to expand care management services to non-value-based lives, it does make sense if the goal is different outcomes. Different outcomes, come from doing things differently. If the desired outcome is to move to full risk, to achieve the financial flexibility that providers want and need to care for a heterogeneous population with increasingly complex conditions and comorbidities, it will require investing in success every single day and with every single patient. Population-based care management is that investment.
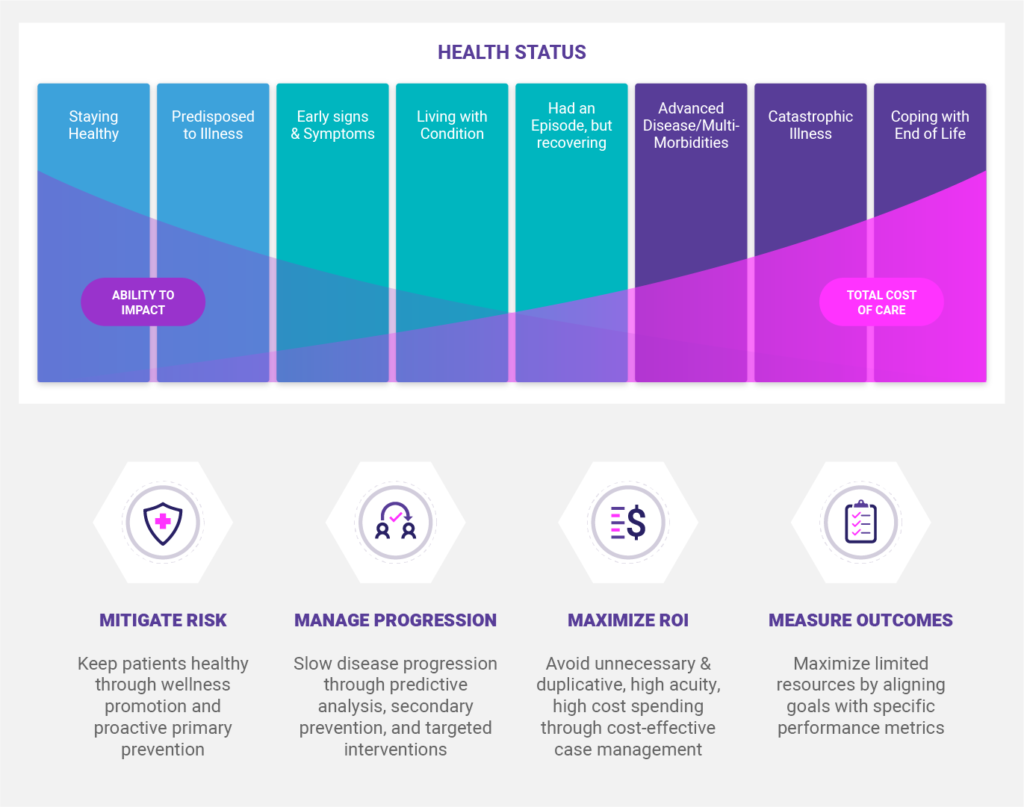
Why? First, the fluidity of risk across populations will result in roughly 18 – 20% of the moderate /rising risk patients progressing to a high-risk status. This will require increased staffing year over year until it becomes unsustainable. Second, the “Ability to Impact” patient outcomes and costs is greater at the beginning of an illness. As time goes on and the disease progresses, it becomes more difficult to effect change both on a population and patient level. Ideally, the focus would be to target interventions on the moderate/rising risk populations to attain optimal returns. Lastly, to achieve the triple aim, initiatives must include promoting wellness and primary prevention otherwise Population Health is a pipedream.
A population-based care management approach applies care services across the full continuum of health and healthcare, with the goal of providing appropriate interventions based on the patient’s current health status and unique needs. It focuses on four core objectives:
- Mitigate risk by keeping patients healthy through wellness promotion and proactive primary prevention.
- Manage disease progression through predictive analysis, secondary prevention, and targeted disease interventions.
- Maximize returns by avoiding unnecessary & duplicative high acuity, high-cost spending through cost-effective case management.
- Measure outcomes using a consistent strategy that aligns system goals with specific performance metrics.
Achieving Population-based Care Management through Integrated Data & Analytics
Succeeding under this type of care model requires a new level of precision, one that can only be achieved through quality comprehensive data, predictive analytics, timely business intelligence, and thoughtful program planning. A well-designed population-based care management program powered by the right technology can assist organizations in reducing unnecessary utilization; avoiding costly events; improving patient outcomes and population health; and reducing per capita healthcare costs. The key to all of this, of course, is building a strong technology core that can power all of the needed components for delivering personalized interventions. To learn more about care management analytic frameworks and how Inflight Health is advancing a population-based approach, book a call with a member of our success team.