The purpose of the Emergency Department (ED) is to save lives by providing immediate care for individuals with life-threatening conditions. Over the past 2 decades, the U.S. has seen an increasing abuse of EDs for conditions that could be avoided if better managed in physician offices, clinics, and urgent care centers. The latest reports from the CDC indicate there are roughly 130 million ED events that occur each year of which 13% to 27% are preventable and could be managed at less acute/less costly sites of services. This is leading to overcrowding in the EDs and creating a significant financial burden on the economy, healthcare system, and consumers.
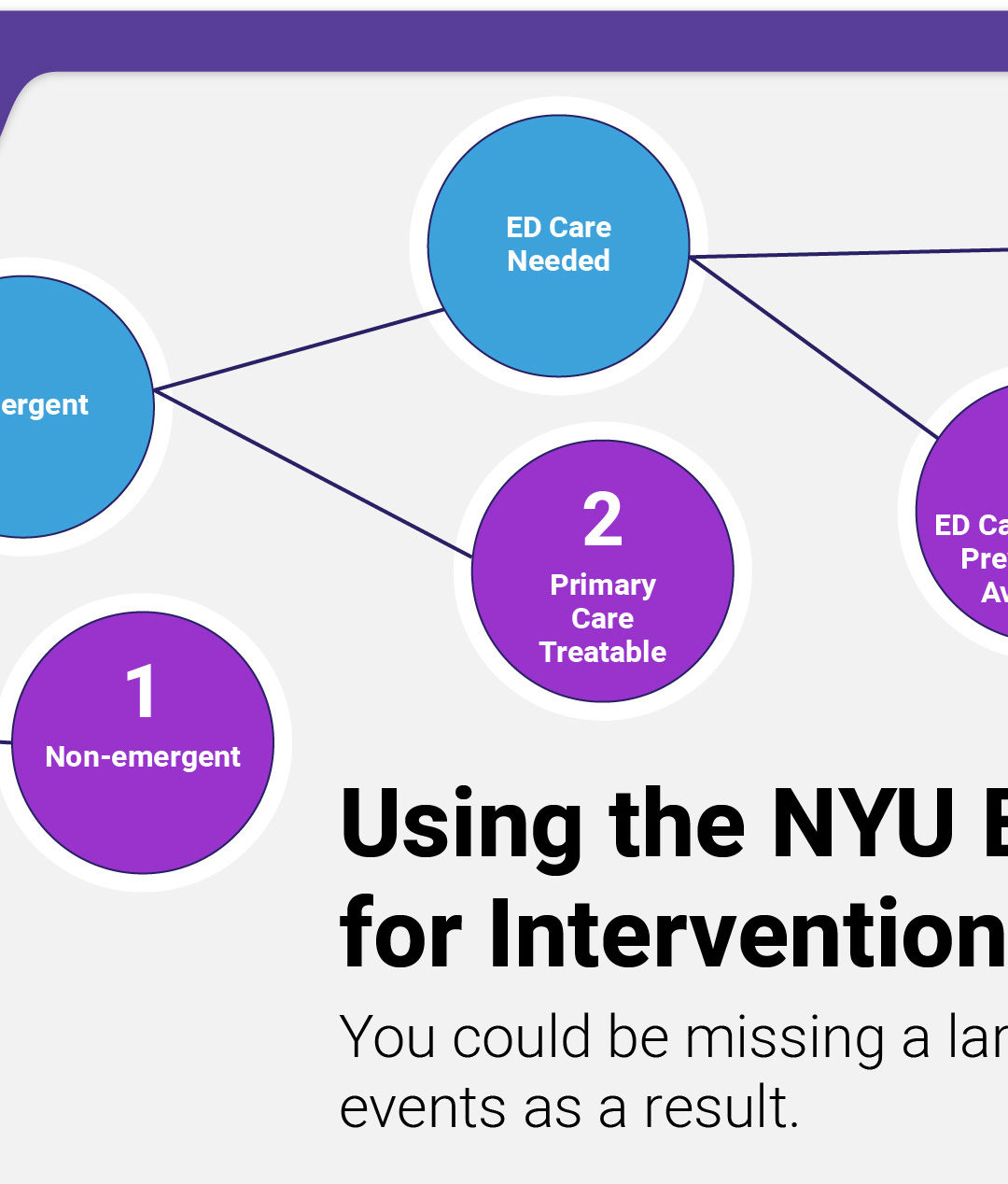
Efforts to reduce preventable ED visits continue to be an industry focal point. Many advancements have been made over the years to identify these events in the hopes of improving care management/coordination, access to primary care, and health literacy. The most notable tool in use would be the NYU Emergency Department Visit Algorithm (NYU-EDA). This is by far the most widely used model for classifying and assessing ED visits for purposes of research, shaping public policy, and driving intervention efforts.
Limitations with the NYU-EDA
The algorithm was developed in the late ’90s and was based on 5700 ED discharge abstracts from 6 hospitals in the Bronx, NY. The algorithm placed ED visits into 1 of 8 categories: (4) Emergent/non-emergent categories, (3) Mental health categories, (1) Injury category, (1) Unclassified category. While the NYU-EDA has been instrumental across research and public policy, many emergency medicine clinicians argue that the clinical precision of the algorithm is deficient for use in interventions aimed at reducing unnecessary visits or for denying payment; claiming that the algorithm itself has not kept pace with its growing popularity. The two primary concerns of the NYU-EDA have to do with (1) outdated code sets and (2) limited code sets.
Outdated Code Sets
The NYU-EDA algorithm was developed using the discharge diagnosis codes of the International Classification of Diseases, Ninth Revision Clinical Modification (ICD-9-CM) and has not been updated to incorporate the new diagnosis codes into its classification of ED visits, which have been released every year by the ICD9/ICD-10 Coordination and Maintenance Committee.
Limited Code Sets
The NYU-EDA system classifies ED events based solely on discharge diagnoses which do not account for underlying differences in morbidity and access to care that could account for utilization patterns. There may also be reasons for a visit that aren’t captured in a discharge diagnosis.
Improvements to the NYU-EDA
Many researchers and statisticians are working to expand on the good works of the NYU team and to make the algorithm more clinically relevant for use in intervention. A good example of this is the Johns Hopkins University team. Using their best clinical judgment and diagnosis aggregations from the Adjusted Clinical Groups (ACG) system, the team was able to create a more comprehensive algorithm for classifying ED events for retrospective analysis. This is referred to as the Johns Hopkins Emergency Department Algorithm (JH-EDA) which is is available in the Johns Hopkins ACG System. In building out the enhanced algorithm, the team expanded on the codes used by reclassifying and cross-walking it to the latest ICD-10-CM version, which included mapping more than 70,000 diagnosis codes. The team also created additional granularity by expanded injury visits into 3 severity categories making for a total of 11 possible classifications.
An observational study was conducted by the Johns Hopkins University team to validate the JH-EDA. The research connected pairwise comparisons of the visit distributions among 4 EDA versions, including the NYU-EDA, to public use files and hospital billing data for a health plan cohort. They found that the “JH-EDA revised classification has a higher rate of nonemergent visits than the original NYU method due both to the large number of previously unclassified diagnosis codes placed here and to the decrease in the percentage in the ED needed but preventable emergent category due to our class assignment, rather than the probabilistic approach used by the original NYU algorithm”. Additional information can be found in the original article, “A Revised Classification Algorithm for Assessing Emergency Department Visit Severity of Populations”, published in The American Journal of Managed Care.
Due to the expanded code set and additional granularity of injury severity, the JH-EDA is more clinically relevant and appropriate for use in intervention strategies. Using the JH-EDA, the Inflight Health platform provides the expanded capabilities that health systems and provider groups need to classify ED visits for use in care management and provider performance measurement activities. As an example, care teams are able to easily identify patients that are using the ED for potentially avoidable situations that could benefit from closer care coordination and disease management support. Further analysis can be conducted using the Inflight Health platform to understand ED misuse by examining related factors such as care density, medication management, the risk for falls due to frailty, etc. Using this information, care teams can work with the patient to educate, inform, and better coordinate care based on the individuals’ unique needs.
Parting Thoughts
Reducing preventable ED events is a complex problem and while many improvements have been made to enhance the NYU team’s work, most models still remain retrospective looking. To be truly transformational, any model must be forward-looking. Book a call with a member of our team to learn more about how Inflight Health is advancing the fight to end the misuse of the ED through predictive modeling.